Ensuring that all people have access to health services, which are affordable, of good quality and within reach, is a public health imperative. Whether to drive down maternal and child mortality, to halt rising rates of noncommunicable diseases, or to prepare for and respond to public health emergencies, strong, accessible health systems are key to achieving the sustainable development agenda and securing health and wellbeing for all.
Such systems are also critical to beating back the rapid advance of antimicrobial resistance (AMR), a problem caused by mutations in microorganisms that become resistant to drugs. Though the battle against AMR is being fought on many fronts — from optimising the use of antibiotics in the animal and agriculture sectors to investing in research and the development of new antibiotics — increased health coverage remains a powerful tool to counter AMR’s deadly menace and ensure our most precious drugs remain fit for purpose. This is so for a number of reasons.
First, increased access to health services — both prevention and treatment — boosts overall population health and diminishes the spread of infectious bacteria. This is especially important for poor or marginalised populations, many of whom lack adequate sanitation and hygiene and are at greater risk of bacterial infections. Increased access to quality health services may result in the more rational use of antibiotics — a critical outcome given that unnecessary use of antibiotics accelerates AMR. At present, an estimated two-thirds of antibiotics are consumed without prescription, in many cases inappropriately.
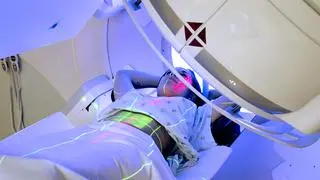
Second, better quality services can decrease healthcare-associated bacterial infections. Infections occurring in health facilities have an estimated prevalence of more than 10 per cent in low and middle-income countries, meaning advances in antibiotic stewardship and infection control — including the provision of adequate water, sanitation and hygiene — can reduce this burden. Also, better quality antimicrobial drugs will help ensure bacteria are destroyed rather than given the chance to mutate, while access to advanced diagnostic tools will help health workers identify and treat infections more effectively.
And third, policies that make healthcare more affordable, including by reducing out-of-pocket expenditure, can help increase access to antimicrobial drugs. An estimated 70 per cent out-of-pocket payments across the region are on medicines, including antibiotics. This makes access to effective treatment unnecessarily costly for poorer people, who may consume incomplete courses of antibiotics, hastening AMR. If accompanied by more stringent treatment guidelines and revised incentive schemes (for example de-linking the payment of health workers from the volume of drugs sold), cheaper antibiotics have significant potential to advance both the UHC and AMR agendas.
Importantly, one of the best ways to achieve this outcome is via the dissemination of high-quality information and advice to health workers and the public. More and better information on the rational use of antibiotics will help health workers treat ailments more efficiently and optimally. At the same time, messaging that persuades the public that antibiotics aren’t the ‘cure-all’ they have come to be known as will help ensure they are sought-out only where necessary, reducing inappropriate consumption and the resistance it breeds.
The writer is Regional Director for South-East Asia, WHO







Comments
Comments have to be in English, and in full sentences. They cannot be abusive or personal. Please abide by our community guidelines for posting your comments.
We have migrated to a new commenting platform. If you are already a registered user of TheHindu Businessline and logged in, you may continue to engage with our articles. If you do not have an account please register and login to post comments. Users can access their older comments by logging into their accounts on Vuukle.