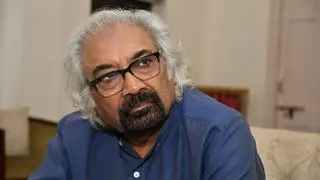
In addition to continuing with the immediate Covid-19 care, the coming budget work towards the goal of allocating 2.5 per cent of GDP on healthcare by 2025 and significantly reducing out-of-pocket expenditure (OOPE) for the lower middle income groups and other vulnerable segments of the population, said K Srinath Reddy, President of the Public Health Foundation of India (PHFI).
“Despite all the things being said, India’s health budget hasn’t increased very much over the years. Even the goal of 2.5 per cent of GDP by 2025 is very modest goal. There you have to look at what the World Bank and the World Health Organisation have been saying. For an efficient delivery of health coverage, the OOPE should not be more than 15 to 20 per cent of the total health expenditure. In India it is at 58 per cent currently,” Reddy told BusinessLine in an interview.
Labour taxes not feasible
In rich countries, there are employer-provided health insurance schemes, with salary deductions. These so-called labour taxes are not feasible in low and middle income countries because a large percentage of the workforce is in informal sector, he said. Therefore, the Centre and the States will have to put up more money as tax revenues. This should ideally come from direct taxes and less from indirect taxes. Because indirect taxes affect the poor too. Direct taxes are related to income and property.
So, even if the government moves towards 2.5 per cent of GDP spend on healthcare, it may not be able to reach the 15 to 20 per cent ideal. As a result, the government may have to continue to raise its funding for healthcare even after reaching the 2.5 per cent target, the PHFI chief said.
Also, there is what is called ‘the missing middle’. Because PM Jan Arogya Yojana covers 40 per cent of the poorest of poor, while 10 per cent of the affluent have their own or employer-provided health insurance schemes. The 50 per cent of the population in the middle is vulnerable. The government could bring them into the fold of the PMJAY by giving them income-graded premium for coverage, even if they cannot give them completely free cover, Reddy suggested.
Link to Health Mission
Also, to reduce the out-of-pocket expenditure the government could look at the possibility of linking the PMJAY with the National Health Mission which in turn can take care of medicines, diagnostics and outpatient services, which are the major cause of high out of pocket expenditure. He said since the States account for two-thirds of the public healthcare spending, the Centre should show them by example.
Reddy agreed that Covid-19 care would be a major immediate focus for healthcare in the forthcoming budget. The government, however, should fund Covid vaccination through extra-budgetary resources. It would also work with the States on Covid vaccination funding as vaccination in an epidemic is for public good. “When I get vaccinated, I do get protection. But along with me 10 others are also protected as I would not transmit the infection,” he said.
“If you are also going to balance all other healthcare needs, your existing health workforce which is already short, whether in terms of ANMs or whether in terms of doctors, you cannot divert all of them only to do covid vaccination. So you need to train many more vaccinators. The expansion of the pool of vaccinators and training programmes would be part and parcel of this year’s agenda,” Reddy said.
The investment for improving the health system over a steady state performance is another area. The budget should focus substantially on creating both rural and urban primary healthcare as priority.
Infrastructure
The focus should also be on strengthening district hospitals, medical college hospitals and emergency transport system. “Because you are still going to be short of people, you have to scale up that a lot,” he said
Since institutions offering medical education are concentrated mainly in southern and western India, much less in central, northern, eastern and north-eastern India, this imbalance needs to be corrected.
“One way one can do quickly is by upgrading district hospitals. The staff in these hospitals can be made into teaching staff, link them up with one or two medical colleges in the region, first start training allied health professionals, nurses and subsequently introduce medical undergraduate and then medical postgraduate degrees. Unless you strengthen district hospitals and transform them into medical training centres, you will not be able to create sufficient healthcare workforce,” Reddy observed.






Comments
Comments have to be in English, and in full sentences. They cannot be abusive or personal. Please abide by our community guidelines for posting your comments.
We have migrated to a new commenting platform. If you are already a registered user of TheHindu Businessline and logged in, you may continue to engage with our articles. If you do not have an account please register and login to post comments. Users can access their older comments by logging into their accounts on Vuukle.